This blog is the first in a series of profiles of different clinical health professions represented by Health Professions Network member organizations. These profiles are intended to give students and those looking at prospective careers in health care an accurate, professional perspective on different health care fields, specialties and careers. "A Day in the Life of a Cardiovascular Technologist" was developed by the Alliance of Cardiovascular Professionals, an HPN member organization.
Table of Contents
- What is a Cardiovascular Technologist?
- Cardiovascular Specialties & Work Environment
- Goals and Rewards of Being a Cardiovascular Technologist
- Becoming a Cardiovascular Technologist: Educational Programs
- Cardiovascular Technology: Professional Outlook & Salary
What is a Cardiovascular Technologist?
Cardiovascular technology is a field of study and practice in cardiology, a field of medicine focused on the heart and vascular system. Cardiovascular technologists are allied health professionals who work closely with and assist cardiologists, physicians and nurse practitioners who specialize in cardiovascular health. Cardiovascular technology has a number of sub-specialties which reflect sub-specialties in cardiology—specialties such as Invasive, Non-invasive, Echocardiography, Electrophysiology, and Peripheral Vascular—which have overlapping knowledge requirements but different day-to-day responsibilities.
Narrowly, one might think of a cardiovascular technologist as a professional educated specifically for cardiovascular technology and qualified by a credential, through an organization like Cardiovascular Credentialing International, for example. But radiologic technologists, diagnostic imaging professionals who specialize in radiography, may also work in cardiovascular technology and be considered cardiovascular technologists—and both cardiovascular and radiologic technologists will likely work alongside registered nurses specializing in the same work environments. Each of these professional backgrounds has different educational curriculae and experiential requirements, which means that all of these professionals, along with cardiologists, bring unique experience, perspective and knowledge bases to the field of cardiovascular health.
This profile will focus on the more narrow definition of cardiovascular technologists educated and credentialed independent of the fields of radiologic technology and nursing—as the fields of nursing and radiologic technology will be covered extensively in other professional profiles.

Cardiovascular Specialties & Work Environment
While all cardiovascular professionals need to understand principles and specifics of monitoring cardiovascular health, a day in the life of a cardiovascular technologist may look very different depending on their specialty. These specialties represent different opportunities and career paths for prospective cardiovascular professionals—and often, educational programs will be specific to a particular specialty.
Invasive (Cath Lab) Cardiovascular Technology
SHOW MOREInvasive cardiovascular technologists are integral members of the cardiac catheterization laboratory team—an environment where diagnostic and therapeutic procedures are undertaken intravenously. Cardiac catheterization, the threading of a catheter into patients' veins to the heart, is minimally invasive compared to open surgery, but still involves a sterile, invasive environment where technologists are required to "scrub in" to the procedural laboratory. Depending on the cath lab, procedures may be largely pre-scheduled, routine and/or diagnostic, but cath labs may also be used in an emergency capacity to quickly treat patients experiencing a heart attack, for example. Technologists may take a number of rotating roles in this environment—sometimes scrubbing in to prep the patient and assist the invasive cardiologist, directly, and sometimes working in a removed, monitoring role, assessing the patients' vital signs and real-time diagnostic data.
The Cath Lab team gathers for our morning huddle; we discuss any issues that came up the day before and talk about the upcoming day—a case at 0800, another at 0830. The schedule doesn’t look too bad. All of a sudden, four beepers go off. It’s the sound of... an ST elevation myocardial infarction. Like clockwork we prepare for the case—entering orders into the computers and x-ray equipment, preparing meds, prepping the procedure tray. Our patient arrives from the ED. He’s 42 years old, pale, diaphoretic, and scared. Despite receiving medication to control his chest pain, he’s an eight out of ten on the pain scale. As we move him to our procedure table, he whispers, “Don’t let me die.”
A Day in the Life: The Cardiac Cath Lab - Anne Arundel Medical Center Nursing Blog, September 2010
Electrophysiology (EP Lab) Cardiovascular Technology
SHOW MOREElectrophysiology (EP) is a specialty that has some overlap with the invasive specialty, as electrophysiology procedures may occur in the catheterization laboratory environment, but often healthcare organizations maintain dedicated EP laboratories for electrophysiology-specific procedures. Electrophysiology technologists specialize in the diagnosis and treatment of heart rhythm problems—requiring the implantation of pacemakers, for example. The EP lab is a similar environment to the cath lab, though the procedures—and required knowledge and experience—are different.
We prepare our room, and although it would be nice to have a few more minutes of downtime, our patient arrives. A short time later, we have sheaths placed and Dr. Bello is trying to get the CS catheter positioned. However, despite trying every angle imaginable, Dr. Bello is having no luck... Not having CS catheter access, this case is going to be a little more challenging... We get the ablation catheter positioned in the left atrium and begin searching for a pathway potential. Finding some interesting electrograms, Dr. Bello asks Nicole to get ready to start ablating. Almost as soon as Dr. Bello applies his first ablation lesion, Melissa at the monitor exclaims, “Hey, do you see that?” Our delta wave disappears and is replaced with a beautiful sinus beat. Having expected this to be a tougher case, Dr. Bello turns around with a smile on his face and says, “Who’s your daddy now?” We all burst out laughing together.
A Day in the Life of an EP Tech - EP Lab Digest, October 2009
Echocardiography / Cardiovascular Sonography
SHOW MOREEchocardiography (Echo) technologists or cardiovascular sonographers are, by comparison, non-invasive specialists largely focused on the diagnostic performance of echocardiograms and the evaluation, rather than direct treatment, of heart disease. Ultrasound images are often associated with pregnancy, but Echo technologists use ultrasound equipment to gather data about and evaluate the structure and function of the heart. Echo technologists may work one-on-one with patients performing diagnostic ultrasounds and stress testing, where ultrasound is used soon after the patient is active on a treadmill or stationary bike.
After taking off your coat and setting down your morning coffee, you begin to review the patients that cardiologists have scheduled today for an ultrasound (echo)... You hope that today’s patients will arrive on time, because this helps you to stay on schedule and enables you to devote at least a little time to helping each patient feel calm and comfortable before the echo... You may be called by an emergency room doctor to perform an ultrasound for a patient suspected to have had an aneurysm. Since the patient is not stable and cannot be transported to the imaging department, you must transport the ultrasound equipment to the patient in the ER exam room. You perform the ultrasound and then call into the cardiologist, who examines the results, consults with the doctor in the ER, and confirms whether the patient requires immediate surgery.
A Day in the Life of a Cardiovascular Sonographer - American College for Medical Careers Blog, July 2017
Non-invasive Cardiovascular Technology / Peripheral Vascular
SHOW MORENon-invasive may be used as a catch-all term to describe specialists in all non-invasive diagnostic cardiac testing, including echocardiography and electrophysiology outside of invasive environments. As such, non-invasive and peripheral vascular technology are recognized as distinct specialties, but they may also be grouped together, depending on the organization or educational program. Peripheral vascular technologists evaluate blood flow in the arteries and veins all over the body—in the patients' legs, for example—rather than just the heart, monitoring blood pressure and also using ultrasound to determine where there are blockages. Like Echo technologists, non-invasive and peripheral vascular technologists may work largely in a one-on-one capacity with patients and perform stress testing.
You will be analyzing about a million cardiograms every day. You will often be doing stress tests, and even Holter scans, likely. I have found that most times, everything is by the book, with no major surprises to worry about. I like that this job (while in a very stressful environment) is pretty stress free... Well, there is still quite a bit of action every day of work. You could be doing four calls to the emergency department on a lunch break. You could be guiding the public out of the way so emergency personnel can get to a patient in need. You could be consoling a patient who is in the worst pain of their life. All these things I have done already (before beginning my practicum mind you!)
A Day in the Life of a Cardio Tech - Stenberg College Cardiology Technologist Blog, April 2015
Goals and Rewards of Being a Cardiovascular Technologist
The Alliance of Cardiovascular Professionals surveyed a wide range of members to offer their perspective on the personal and professional rewards of being a cardiovascular professional.
These professionals serve a vital function in all areas where they practice, because their specialized education and training provides invaluable diagnostic and interventional support to cardiologists and radiographers. All cardiovascular professionals we spoke to find fulfillment through their role in improving patients' healthcare experience as well as, of course, their health.
Few things are more rewarding than seeing a patient in the midst of a heart attack, ashen grey and writhing in pain, become relaxed and pain free when an occluded coronary artery is opened.
Managing the Patient Interaction
SHOW MOREA cardiovascular professional is generally a key person in managing the patient interaction and is the cornerstone for ensuring a relaxed, satisfied and safe patient. Cardiovascular professionals often introduce patients to particular procedures, explain the process, and answer the patients' questions, providing reassurances and offering calming support. This is a core competency, especially in environments where cardiovascular technologists work in a one-on-one capacity with patients.
My goal was to make the patient as comfortable as I could. Many patients were afraid or just had questions. Answering these questions usually put them at ease. Most patients appreciated being included in the conversation going on while getting them ready for the procedure.
Depending on the procedure, patients may be acutely ill or otherwise uniquely worried about their health. Fear is a common denominator. It is well-documented that fear compounds illness, so the cardiovascular professional's role in calming patients and assuaging fear is crucial to the most successful healthcare outcomes. Professionals often measured their personal success based on the calmness of the patient!
Smiles – nothing can make you feel better than to see a smile on a patient’s face.
The Professional's Crucial, Dual Role
SHOW MOREAll of the directors, leaders and educators we surveyed made it clear that cardiovascular professional has a dual role of both providing comprehensive and experienced support and assistance to the attending doctor while at the same time providing comfort, education and care to the patient. Patient satisfaction is often an indicator that the cardiovascular professional is fulfilling this second role effectively.
Doing the best possible test for the patient and telling them that I am treating you like 'my own family member'... Bottom line: I take great pride in my work and try to do whatever is necessary to do a good exam, satisfy the patient and also satisfy the account.
Working & Skill-building as a Team
SHOW MORETeamwork is also a crucial competency and rewarding factor of the work. All cardiovascular professionals we surveyed expressed that their work was significant from both a team and individual viewpoint for impacting the quality of care for patients. With their highly specialized education and role, a cardiovascular technologist is an integral part of a care team made of professionals who may all have different backgrounds and specialties. It is the multi-disciplinary nature of cardiovascular care that creates a unique bond and team approach that values and supports all participants on the team with no one person being better, superior or more valued!
There are several specialists working on the team, not one of them is more important than the other. Each specialist brings an important contribution to the team. I believe that to be the best team member, you should strive to learn as much as you can about all team specialties. This strengthens the team and creates a safer work environment. It’s nice to hear a team member say 'got your back!'
As contributing to the quality of care was particularly important to cardiovascular professionals, continuing education, advancement and participation in a wider network of cardiovascular professionals was a critical goal for those we talked to. Professionals saw the best way to advance quality in their work was to develop their own skills and expertise through greater understanding, skill building and advancement opportunities to improve their own work and help serve as mentors for newer entrants into the field.
I would have to say my greatest reward is that I still love my job and look forward to coming to work each day. In addition, I also value the relationships I have made with members of the profession from across the country. There have been so many people who have helped me in my career that I cannot begin to repay them. My only hope is that I can, in some small way, pay it forward to those that come behind.

Becoming a Cardiovascular Technologist: Educational Programs
Each sub-specialty of cardiovascular technology has a similar-but-not-identical education pathway to certification and/or licensure and eventual employment. Cardiovascular invasive specialists (CIS), electrophysiology (EP) professionals, echocardiography (Echo) technologists, and non-invasive/peripheral vascular specialists each have different clinical, academic, and practical requirements.
Every cardiovascular technologist regardless of sub-specialty will have to complete some combination of formal classroom education, hands-on clinical training, examination / certification, and accredited continuing education after certification has been achieved. Specific academic programs can take anywhere from six months to four years to complete, depending on students’ prior knowledge, training, and qualifications. Typically, cardiovascular technologists complete two-year associate's degree programs, which spend the first half of the curriculum exploring core subjects like biology, anatomy, and physiology, and the second half going into detail in whatever sub-specialty the student selects.
Prerequisites change institution to institution and program to program, but typically prior educational learning in anatomy/physiology is preferred, and participation in the clinical component of the program is dependent upon student academic performance in preceding sections of the curriculum. Additionally, before students can participate in the clinical setting, they often have to be cleared by a background check, drug screening, and physical examination.
The clinical portions of the curriculum allow students to fully understand what their responsibilities will be once they enter the workforce. Some programs make an effort to expose students to different kinds of treatment environments and organizations—a large city hospital vs. a small community hospital, for example, which will have different practical realities and workflows for professionals.
Invasive Education: Perspectives
SHOW MOREWe start from the beginning just taking classes that are more book work, learning the basics of anatomy, and what the heart does for our bodies. Then we take a short two week clinical [course], going to the hospital and getting experience working with patients, doing EKGs stress tests, exploring the electrical side of things to see how the heart works in the body and so on. Then we have more classroom work, learning about hemodynamics and physiology. We do in-classroom clinical skills training and assessment prior to actually going to assist in the hospital. We start with the basics – hooking [the patient] up to an EKG machine, circulating around during the procedures to check equipment readings and see if the physician needs anything, etc. Then we start scrubbing for hands-on participation, assisting the doctor and participating in interventions. Then we’ll take the RCIS exam right before or right after graduation, and start applying for jobs.
– Victoria Johnson, Howard Community College
Non-Invasive Education: Perspectives
SHOW MOREI didn’t realize how long it was going to take to gain the skill of actually being able to find images. It’s a lot harder and more involved than just putting the probe down on the chest. And then academically, too, I didn’t realize how in depth we have to learn the cardiovascular system before we would actually be able to begin work. [Echo techs] start off taking 4 classes, and the schedule is very heavily academic. [The program] is basically just preparing us with all the cardiovascular knowledge we need prior to going to clinic. And then eventually they phase out classes, and by the time you graduate you’re really spending all of your time in the clinic, and studying and practicing for your boards.
- Gracie Welch, Echo Student at Gwinnett Technical College
I chose to go into cardiovascular sonography, honestly, because it’s really efficient. Rather than having to go for this big 4-year degree or do a residency, imaging is nice in that you complete a relatively quick plan of study in two years, and immediately go in to the field and start working with patients. Having been in college before I knew school would be challenging and require organizational skills, people skills, all of that. What I didn’t anticipate was the orthopedic difficulties that you face in sonography. You have to coordinate muscle tone, and stuff like that. I mean you really have to work out to be a sonographer. The reality is that whether it’s the knowledge-based aspect of the job, or the physical aspects of the job, they’re both challenging in unique ways.
- Tyler Farr, Sonography Student at Gwinnett Technical College
Cardiovascular Technology: Professional Outlook & Salary
The U.S. Bureau of Labor Statistics (BLS) maintains categorical data regarding job outlook and salary for Diagnostic Medical Sonographers and Cardiovascular Technologists and Technicians. This is an excellent and premier resource for job outlook information that provides a great picture of the field as a whole, but this categorization includes cardiovascular technicians which are lower, entry-level positions that do not require as much education and experience as cardiovascular technologists. The median statistics, therefore, may be lower than could be expected for diagnostic medical sonographers and cardiovascular technologists, alone.
It should also be noted that BLS data is not segmented regionally, and geography has a significant impact on wages. The Alliance of Cardiovascular Professionals conducted a wage survey in 2017, the results of which are summarized in a report for members-only, though we'll share some of our insights in this resource.
Outlook: The BLS suggests that this field will grow 14%, classified as much faster than average over the ten year period from 2018-2028, expecting 18,000 new jobs to be created in the field.
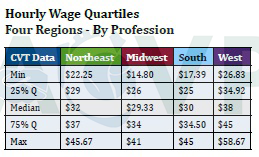
Median Pay: The BLS suggests the median annual wage for cardiovascular technologists and technicians was $56,850 in May 2018, or an hourly rate of $27.33. (This hourly rate is calculate based on 52 weeks of 40 hours per week, though this may not be exact in a real-world context with benefits and paid time off.) Our own survey data suggested a higher median pay for cardiovascular technologists of $32 per hour, or $66,560 per year, annualized. Again, we expect this difference to have resulted from a smaller proportion of technicians as opposed to technologists in our data.
Potential for Advancement: Extrapolating from our data and professional feedback, we interpret salaries in the 75% quartile of our data to be reflective of experienced, senior-level technologists. These senior technologists had a median pay of approximately $36 per hour or $75,000 annualized. We also interpreted the "Max" quartile to be reflective of cardiovascular service line directors and leaders. These professionals who have advanced to management roles in the field earn up to about $50 per hour, or $104,000 per year. Region had a significant impact on wages, so these amounts may be higher or lower depending on where you are located.

